Barrett’s Esophagus
What is Barrett’s Esophagus?
Barrett’s esophagus, also known as Barrett’s disease, is a disorder in which perpetual exposure to stomach acid causes injury to the cells of the lower esophagus. Left untreated, Barrett’s esophagus raises a patient’s risk of developing esophageal cancer by up to 80 percent.
What Causes Barrett’s Esophagus?
Patients with gastroesophageal reflux disease, or GERD, are more likely to develop Barrett’s esophagus than those in the general population. Also known as acid reflux, GERD is a condition in which stomach acid regularly washes back up into the esophagus. To protect their long-term health, patients with GERD should undergo testing for Barrett’s esophagus.
Symptoms of Barrett’s Esophagus
For many patients, Barrett’s esophagus causes few if any symptoms. However, some individuals with Barrett’s disease (or GERD) may experience:
- Difficulty swallowing food
- Chest pain
- Pain in the upper abdomen
Anyone experiencing these symptoms should not hesitate to make an appointment with a board-certified gastroenterologist like Dr. Peyton Berookim.
Risk Factors for Barrett’s Disease
Because many Barrett’s cases are asymptomatic, it’s crucial that patients be cognizant of the risk factors associated with this condition. The following may increase a patient’s chance of developing Barrett’s disease in the future:
- Chronic heartburn / acid reflux
- Smoking
- Family history of esophageal cancer
- Gender (Men are three times more likely than women to develop Barrett’s.)
- Age (Though Barrett’s is more likely in older patients, it can occur at any age.)
- Race (Caucasians have a higher risk of developing the disease than individuals of other races.)
In patients with Barrett’s esophagus, the altered cells in the esophagus can become abnormal. This condition is called dysplasia. Cells with high-grade dysplasia are more likely to become cancerous. The following risk factors may increase a patient’s chance of developing dysplastic Barrett’s esophagus:
- Continued exposure from acid reflux
- Long segment Barrett’s
- Family history of Barrett’s
Undergoing regular evaluation by a gastroenterologist is the best way to reduce your chances of developing dysplastic Barrett’s and esophageal cancer.
Diagnosing Barrett’s Esophagus
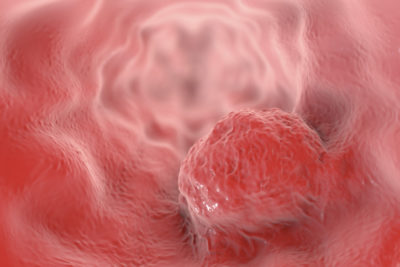
Dr. Berookim performs upper endoscopies and other procedures to diagnose Barrett’s esophagus. During the endoscopy, Dr. Berookim will slide a lighted tube into the esophagus. Using the camera on the end of the tube, the doctor can visualize the lining of the esophagus and identify abnormalities. Whereas the tissue in a healthy esophagus appears pale and glossy, the esophagus looks red and may resemble intestinal lining in Barrett’s patients. Dr. Berookim may also perform a biopsy of the tissue in the esophagus to test for abnormalities.
Treating Barrett’s Esophagus with Radiofrequency Ablation Therapy
In the past, Barrett’s patients had fewer treatment options from which to choose and were often told to wait and see if their condition would progress to esophageal cancer. Fortunately, today’s Barrett’s sufferers have much better options available to them.
While radiofrequency ablation therapy has been used to treat Barrett’s esophagus for a while now, the HALO System affords surgeons far greater control. Using a HALO ablative catheter, Dr. Berookim can precisely remove damaged esophageal tissue without injuring surrounding healthy tissue.
Learn more about radiofrequency ablation and how it can help preserve the esophageal health of Barrett’s patients.
Contact Dr. Berookim: Co-director of the Barrett’s Center of Excellence at La Peer Health Systems.
If you’re suffering from GERD, or think you may be at risk for Barrett’s disease based on your symptoms or risk factors, then you shouldn’t hesitate to schedule an appointment with Dr. Berookim. Monitoring and treating Barrett’s now is the best way to protect yourself from developing esophageal cancer in the future.

